A lot is being decided in the way of potential treatments right now. And as you’ll read here, the decisions are profoundly complex. As you know from the last blog, the critically important issue for Logan at this moment is to try to find a way to recover his bone marrow production and return his immune system. On Tuesday, the results of the bone marrow biopsy came back. Then on Wednesday an interdisciplinary team of doctors from the bone marrow transplant, liver transplant, oncology, and pathology services met, and I’m told they discussed Logan’s case for over an hour.
Immediately after that meeting, three of the attending physicians came to update Becca and I on the course of action they want to pursue, which was put into action today. It all derives from the results of the bone marrow biopsy. As an initial matter, they did not see any female chromosomal cells within the bone marrow. Based on that, the prevailing theory is that GVHD, or graft vs. host disease—as explained in the last update—is not the main issue causing Logan’s bone marrow to be suppressed. If it were, they would expect to see female cells that came from the donor organs within the bone marrow, as they saw in his skin biopsy. However, there was one very atypical finding from the biopsy, and that was the amount of plasma cells crowding out the bone marrow sample. They do not know what is causing the plasma cell buildup in the bone marrow. Perhaps it’s a result of a an immune reaction to the Adeno virus or Candida fungal infection that Logan is testing positive for. Or maybe its from something else. But whatever the cause, the thought is that maybe the plasma cell buildup is preventing the healthy bone marrow and white blood cell counts from recovering.
The typical standard of care for a patient presenting with completely suppressed blood counts would be immunosuppressive medications aimed at stopping T-cells from attacking the bone marrow. But given the underlying infections that Logan has, the doctors are extremely hesitant to go this route and risk the infections flaring out of control with the additional broad-based immunosuppression it would entail. On Monday, before the biopsy came back, the doctors were ready to start one such treatment, but then after a blood culture came back positive for the return of the fungal infection that Logan has had intermittently for a few weeks now, they scrapped that plan as too risky.
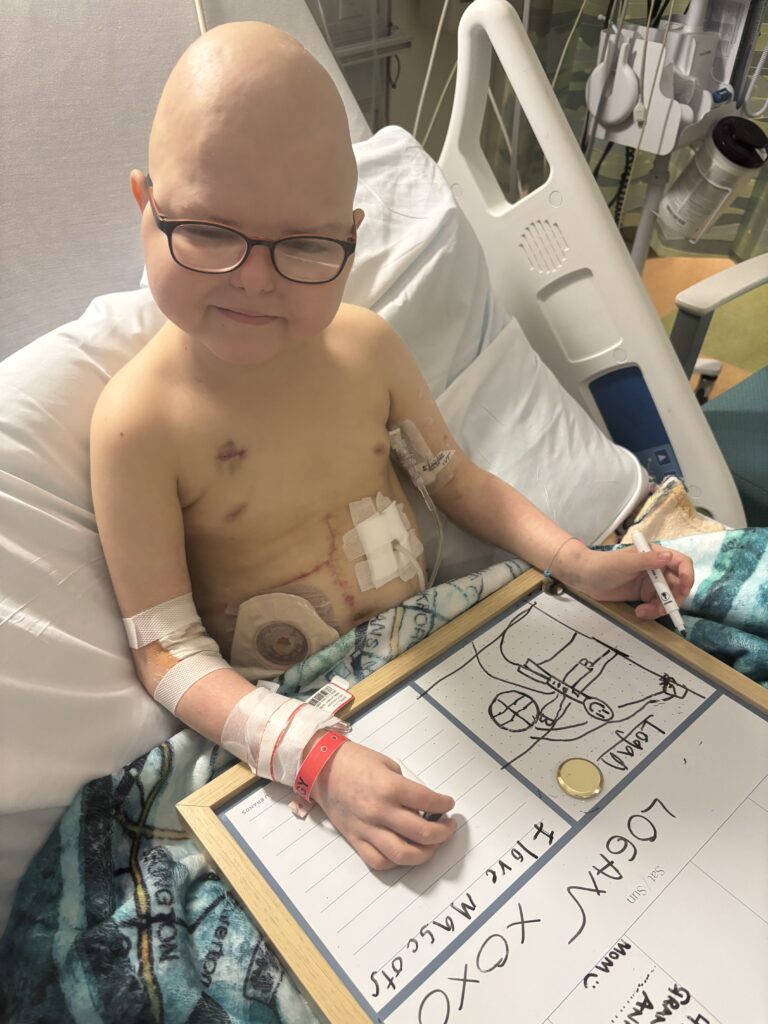
Then the bone marrow biopsy came back with the results showing the high plasma cell concentration. If in fact its these cells interfering with the normal bone marrow and white blood cell production, then it stands to reason that eliminating them could help clear the way for the normal cell growth to return. As such, the doctors today started Logan on a monoclonal antibody medication called Daratumamab that is typically used to treat certain blood cancers. It works by binding in a targeted manner to the CD-38 protein, which is the specific plasma cell that came up in such high concentration in the biopsy. Theoretically, and the doctors are clear this is all theoretical, if that plasma cell buildup is suppressing the bone marrow production, this could provide a very targeted way to eliminate those cells and help to return normal bone marrow production. It would also be less immunosuppressive than the T-cell eliminating agents that were also being considered. The doctors don’t really know if this will work, but we’re praying that it will. Logan needs a break so so bad. They started the first infusion of Daratumamab today. This treatment carries the risk of severe allergic reactions and side effects. Rounds this morning with the doctors and nurses almost felt like a sports pre-game huddle: “everybody is ready right, everyone knows how to handle this or that potential reaction right.” All this to say, no part of this treatment is being taken lightly. They pre-medicated Logan with anti-histamines, anti-nausea meds, Tylenol, and very very high dose steroids to reduce inflammation. The first infusion ran over 7 hours and ended an hour ago, and so far so good. Logan will get another dose tomorrow.
But that’s not all. In addition to the Daratumamab monoclonal antibody treatment, the doctors also decided that a bridge is needed to try to help Logan fight some of the infections until his immune system comes back on line. So they also decided that on Saturday they would like to start giving him direct white blood cell/granulocyte transfusions. This is essentially infusing immune cells directly from a donor into Logan. Although this sounds straightforward enough, it is actually extremely rarely used. We polled the nurses on the floor and couldn’t find one that had actually remembered doing this. Part of it is the logistical challenge. These immune cells are only viable for about 8 hours, so they are harvested from a donor and brought directly to a recipient. They don’t last long in the recipient’s system, but might help to provide an immune boost to help Logan fight the infections until his own immune cells can kick in. Like the Daratumamab, and probably even more so, these transfusions also carry the risk of serious reactions that they will be monitoring very carefully at the time they give the transfusion, and afterwards.
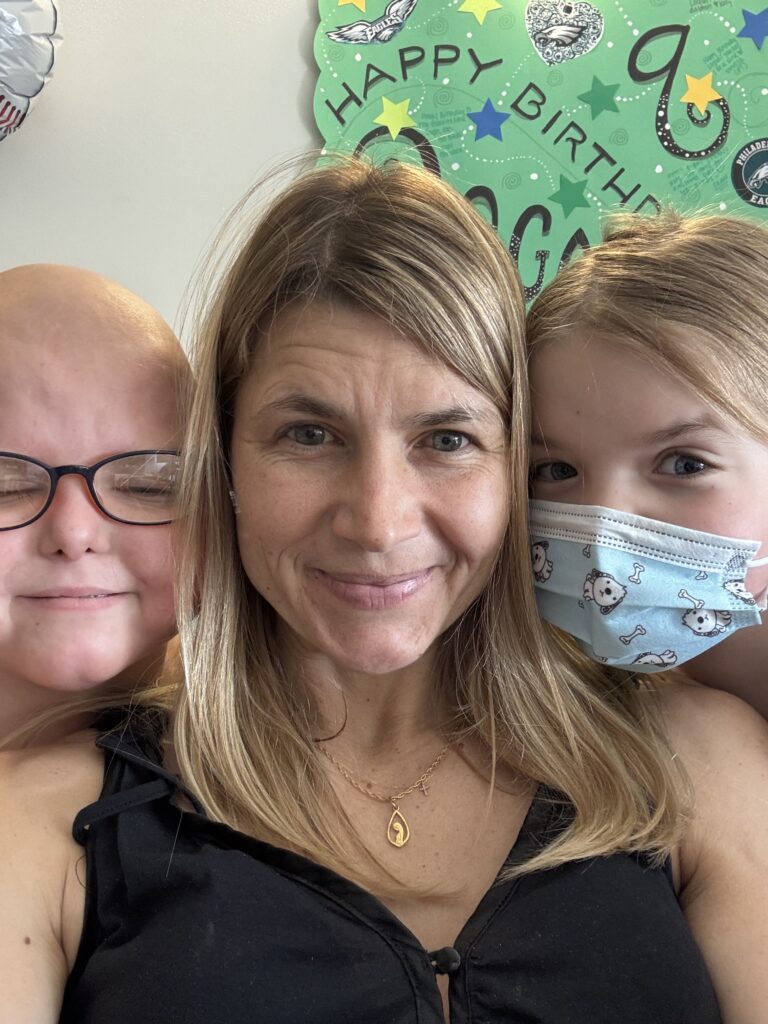
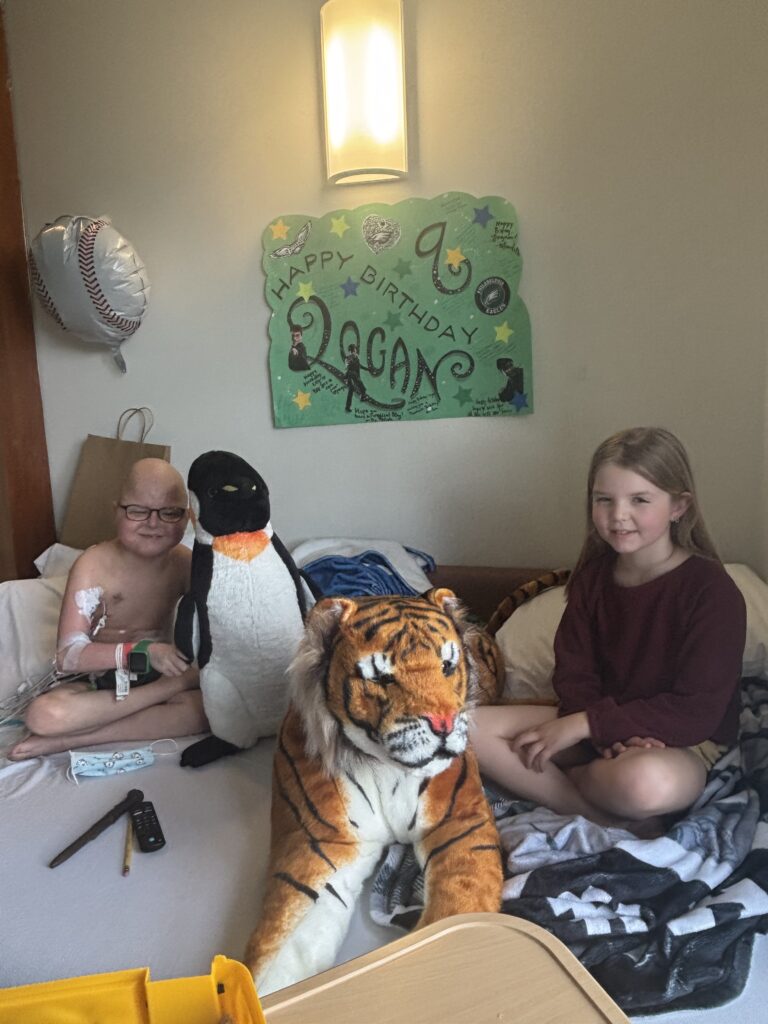
So yes, there’s a lot going on right now, a lot of which is novel and a bit uncharted. Thank you for keeping your hearts behind Logan, and all of us, as he braves this.
More updates to come soon.